digital media
Valve in Valve Mitral Simulator in AR
Augmented Reality allows users to the simulators in a 360-degree view.
In medicine, we are witnessing the emergence of countless highly specialized and complex interventional procedures—procedures that are essential for treating equally complex pathologies. However, the training for such procedures—previously summarized by the aphorism “see one, do one, teach one”—is ethically questionable because the professional has not yet acquired sufficient competence to treat the patient, even under the supervision of a preceptor. Simulator training has been used as a valuable educational tool that, much like in aviation, contributes to the safe acquisition and maintenance of competence for both the professional and the patient.
Simulation as an educational training tool began in 1930 with the advent of the “Link Trainer,” or “Blue Box,” the first flight simulator developed by Link Aviation Devices. At that time, the idea was to teach pilots how to fly an aircraft safely. Since then, simulator training has become an indispensable tool in both civilian and military aviation around the world.

On the other hand, in medicine, simulation training began in the 1960s with a simulator developed by Norwegian plastic toy manufacturer Asmund Laerdal and the Austro-Czech physician Peter Safar. This realistic simulator was originally developed for training in “mouth-to-mouth” cardiopulmonary resuscitation. Over time, this device became known as “Resusci Anne” or “CPR Anne” and is now considered the most widely used simulator in the health field. Subsequently, simulators used in interventional procedures evolved from the simple mannequin model and expanded their range with multiple formats and functionalities.

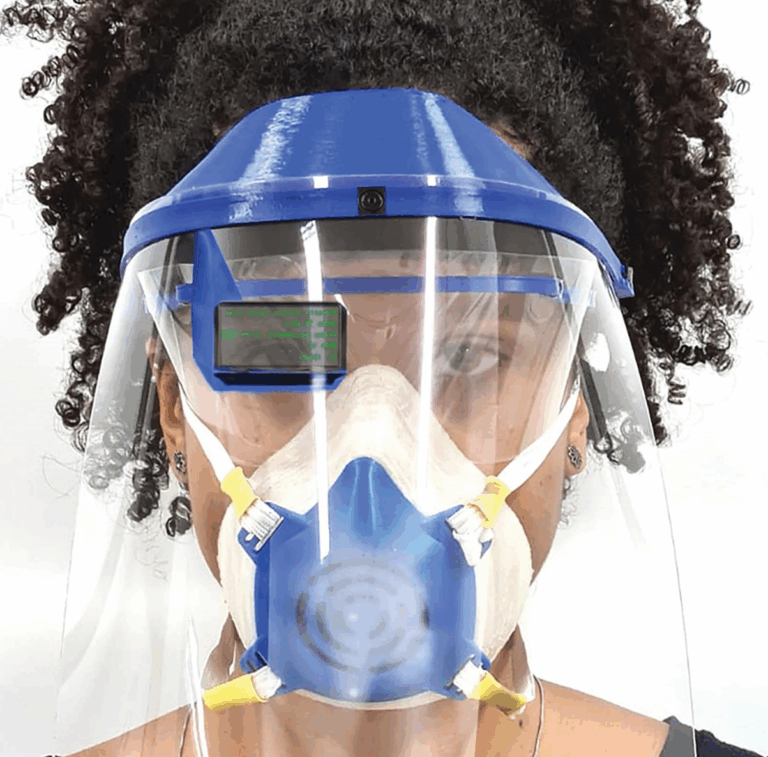
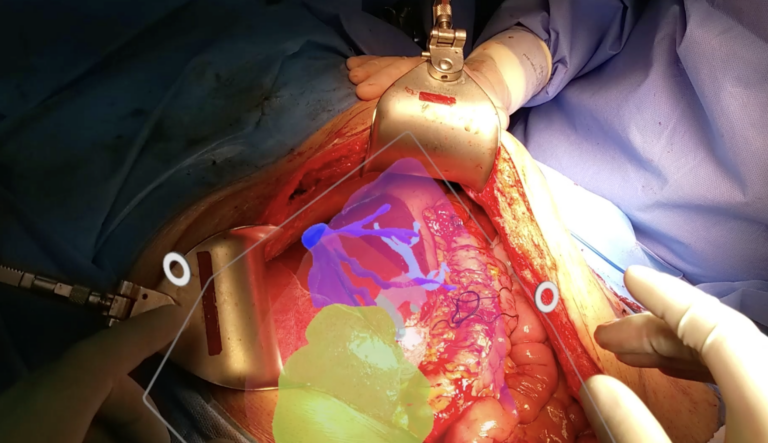
Today, we can, in simplified terms, identify the two main branches of simulation: Virtual Simulation and Realistic Simulation. The first modality includes simulators featuring a virtual patient, where physical sensors—located in a haptic box—are connected to a computer and monitors. In this group, there has also been a progressive advance in the virtual realm, ranging from augmented reality simulators to complete immersion in the metaverse. Meanwhile, realistic physical models include lifelike mannequins and scenarios, bench-top dry simulators, as well as flow simulators.
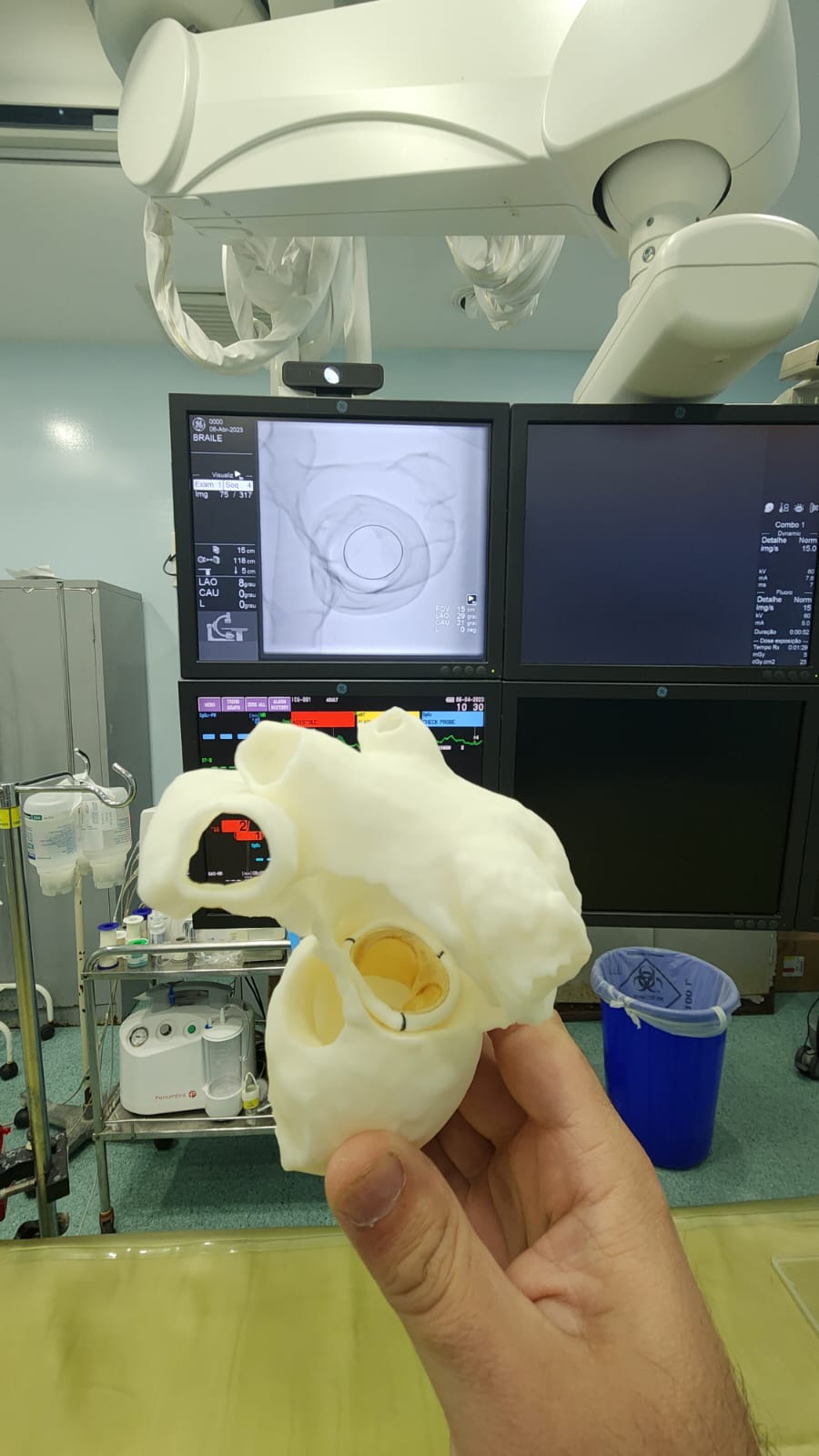
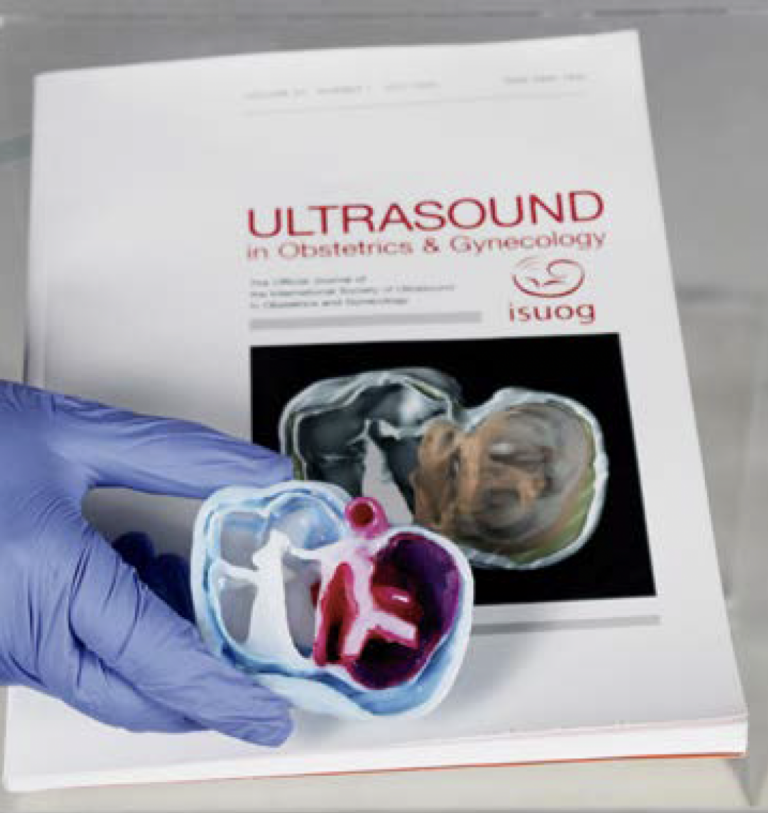
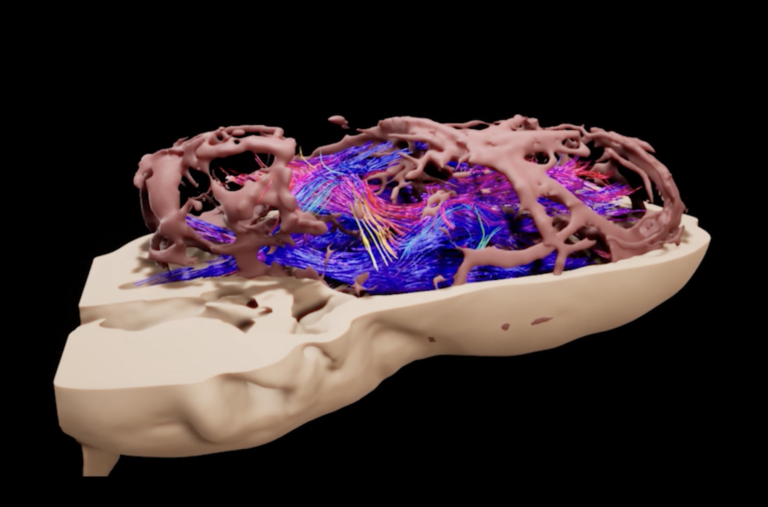
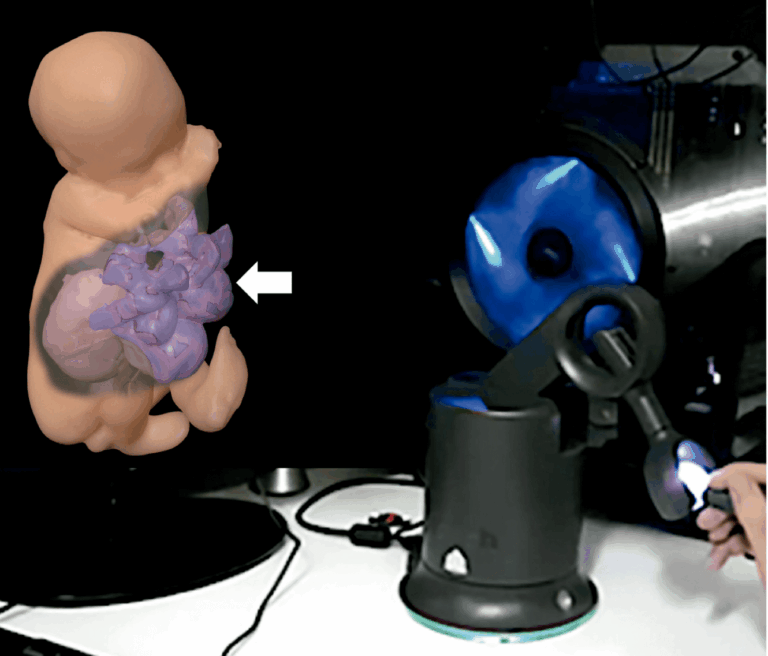
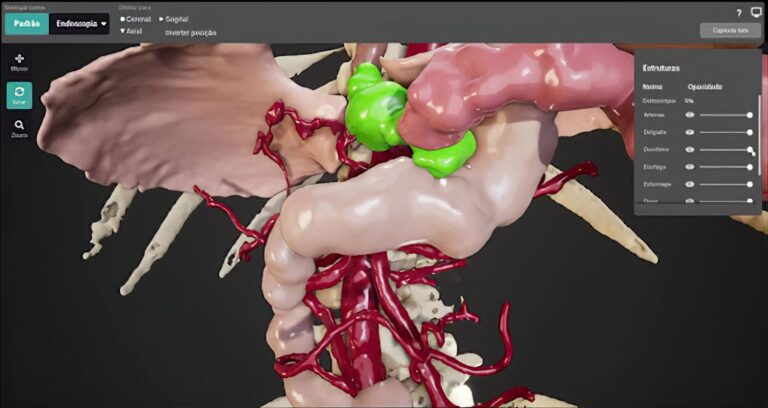
In line with this trend, the BioDesign laboratory at PUC, in partnership with the medical training company SIMULATICS, has been developing realistic physical simulator models based on 3D printing of computed tomography scans from selected patients. The CT scans are segmented to isolate the structures relevant to training. Models for transseptal puncture (performed on the membrane that separates the right and left atria) as well as for “Mitral Valve-in-Valve” (the treatment of a degenerated surgical mitral valve via transcatheter valve implantation) have already been extensively tested and approved in courses, fairs, and conferences in the field of Interventional Cardiology. New models are being developed based on a trinomial of expertise in medical procedures, simulator training, and segmentation with 3D printing.
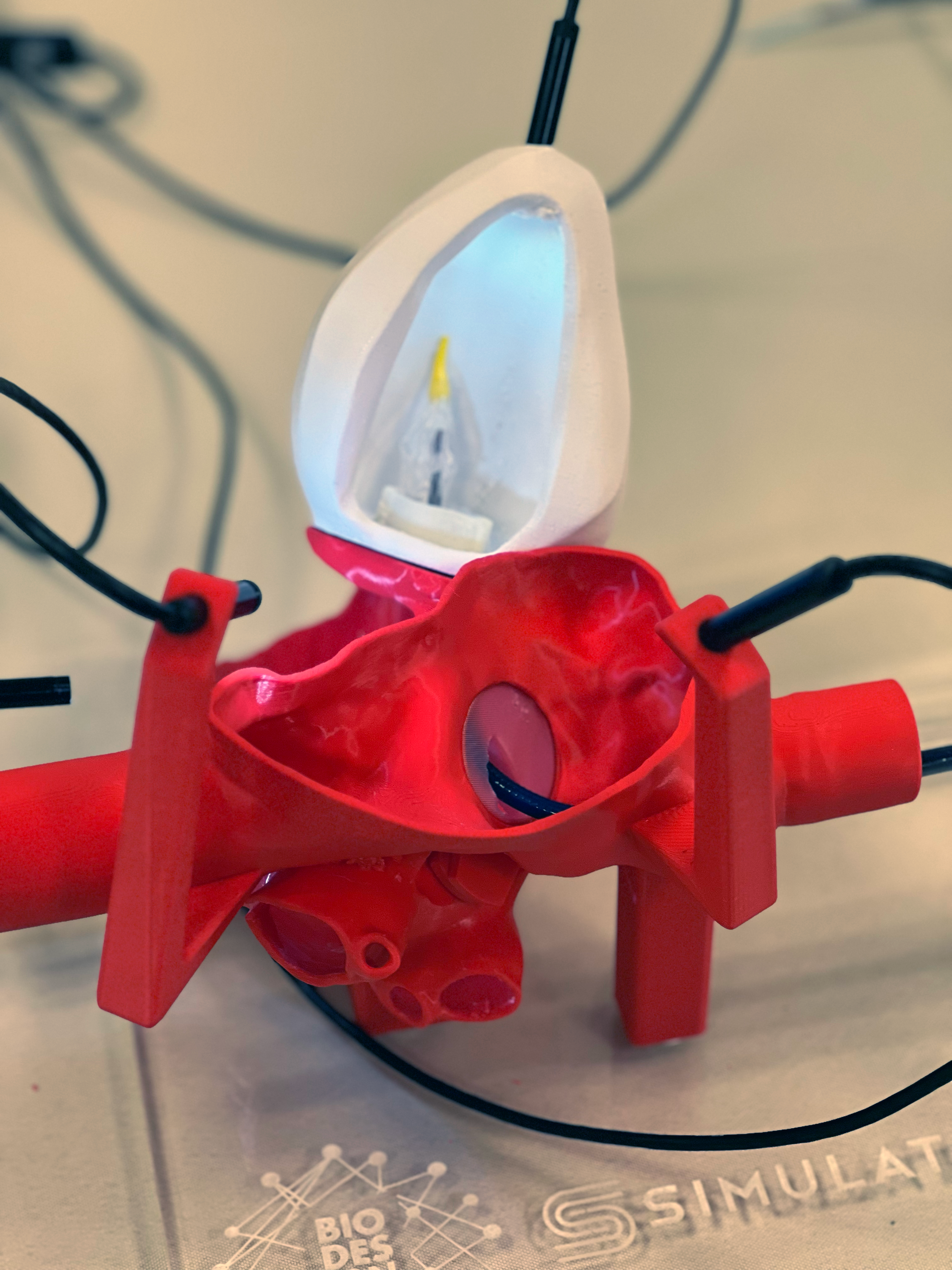



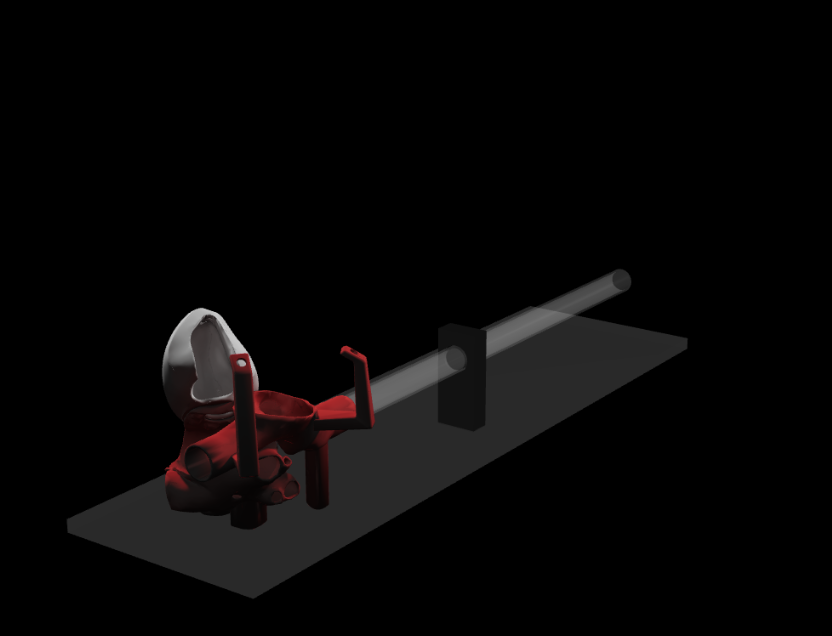
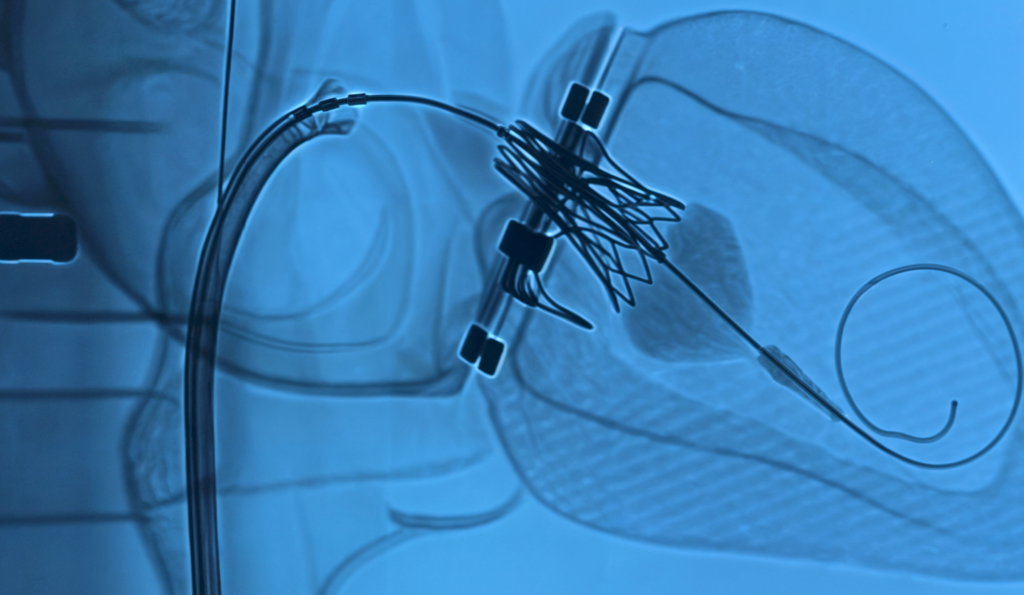
Transseptal puncture is a technique aimed at accessing the left side of the heart through the interatrial septum. By inserting a catheter into the femoral vein, the device is guided to the right atrium, positioned against the oval fossa, and then crosses the membrane, creating a pathway to the left atrium. This approach is particularly relevant in the context of valve-in-valve procedures, which allow the implantation of a new valvular prosthesis within an existing one, thereby avoiding the need for open-chest surgery. The developed physical simulator was designed to replicate these steps, allowing visualization of the structures and providing tactile feedback to the operator.





The development of both Virtual and Realistic simulators serves to meet the training needs imposed by the emergence of numerous interventional procedures. When integrated into a dedicated training curriculum, these devices are educational tools capable of assisting in the acquisition and maintenance of competence in a given activity. The developed simulator demonstrates how technological solutions can transform the teaching of complex procedures. Just as in aviation, interventional medicine seeks to develop training that is both safe and effective for its professionals and patients.
digital media
More on social media