The use of medical 3D models and virtual reality (VR) in pre-surgical planning has been a fundamental tool in surgical strategy and localization for the surgeon, being a situation in which the anatomy is completely divergent from normal standards. VR has also been an important mark, assisting and allowing the surgeon to find the best surgical approach.
Clinical Study 1
(Neurosurgery)
CRANIOPAGUS TWINS
Craniopagus twins (CPT) are an extremely rare malformation in which twins are conjoined at the head. This phenomenon occurs in around 1 in 2.5 million live births. Despite the severity of the anomaly, which is associated with high morbidity and mortality, successful separations have become more frequent primarily due to the constant advances in neuroimaging, neuroanesthesia, and neurosurgical techniques. As regards neuroimaging, there has been great progress, mainly related to the developments in VR and 3D models generated from CT or MRI imaging data. These models have been extremely important in planning surgical strategies and as anatomical references for the surgeon during the procedure.
The first anatomical classification was described by O’Connell, where craniopagus twins were classified as partial or total. Total CPT share an extensive area of the cranial surface with many connections between cranial cavities, while partial CPT share only a small surface of the cranial convexity. The separation surgery in partial CPT is associated with a better outcome than total CPT.
In September 2019, we received eight-month-old craniopagus twins at the Paulo Niemeyer State Brain Institute. They were classified as total vertical craniopagus, presenting an extremely complex anatomy, with a significant circumferential venous sinus and regions of shared brain. They became the biggest challenge of the institution’s pediatric neurosurgery team.
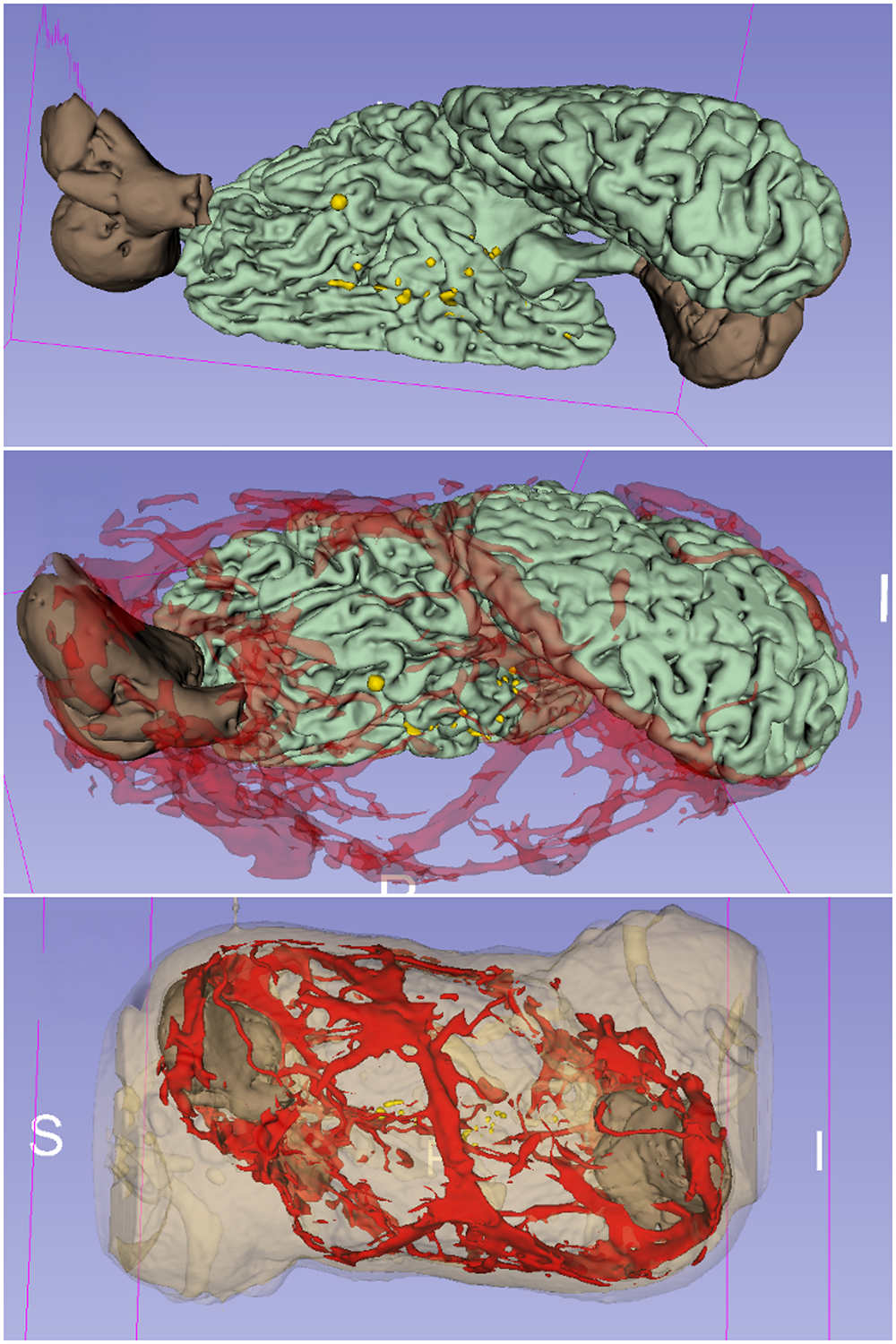
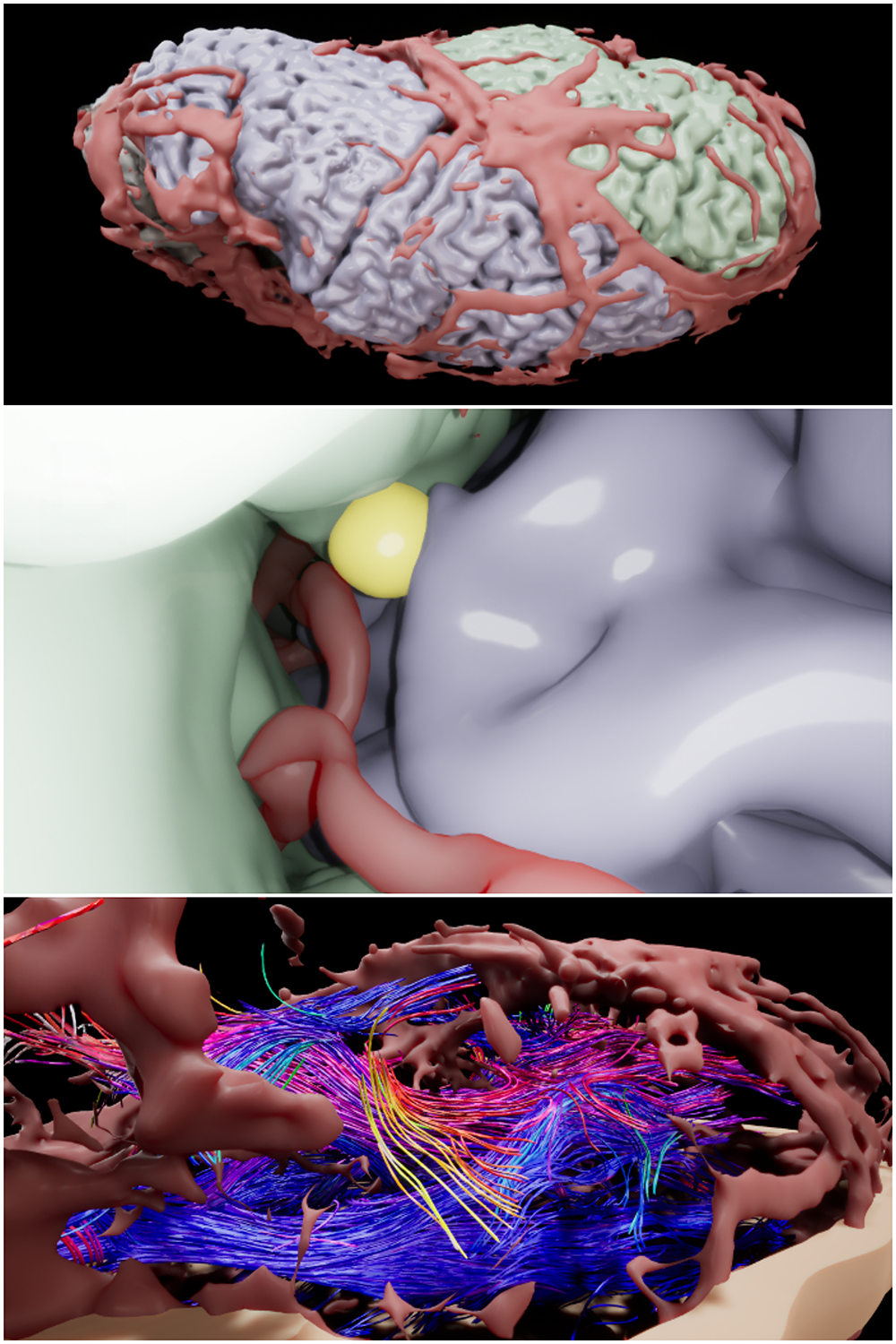

We initiated an elaborate plan with a multidisciplinary group of specialists so as to develop a structure to start the surgical process. For this type of craniopagus, it is crucial to divide the surgery into multiple steps, as a single separation procedure would be impossible. These serial surgical steps are necessary in terms of the development and regrouping of the venous return distribution, given that we must skeletonize the circumferential venous sinus through coagulation of the veins that drain to this sinus. This is done after the analysis by means of cerebral angiography, thus electing the best starting point for the first procedure in a sequence of four or five. In each of these steps, the veins that drain to the circumferential sinus are coagulated, as well as the separation between the twins’ brains. After this separation, a silastic interposition was placed between the separated structures which was kindly donated by Dr. Ricardo Oliveira, Ribeirao Preto USP’s pediatric neurosurgeon, who was present during two of the surgeries and oriented us regarding how to proceed in this complex operation.
In this type of severe craniopagus, it is always necessary to decide, after carefully analyzing clinically and radiologically, which twin to begin on and follow to surgery for partial disconnections. The literature recommends considering initiating the separations on the less favored twin, the one with less chance of survival. In the initial assessment, we concluded that one was clinically and radiologically less favored. This twin was a carrier of cleft palate and presented a significant hemodynamic instability to manipulation.
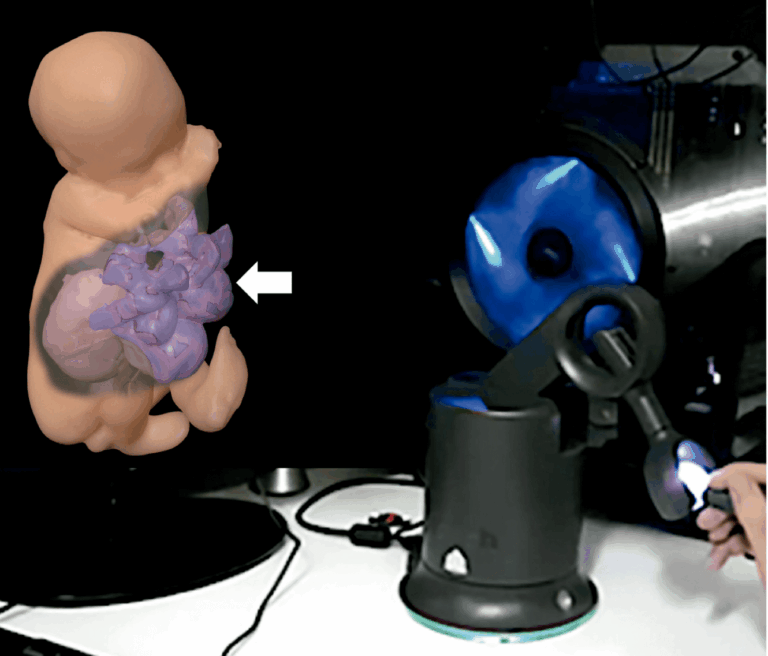
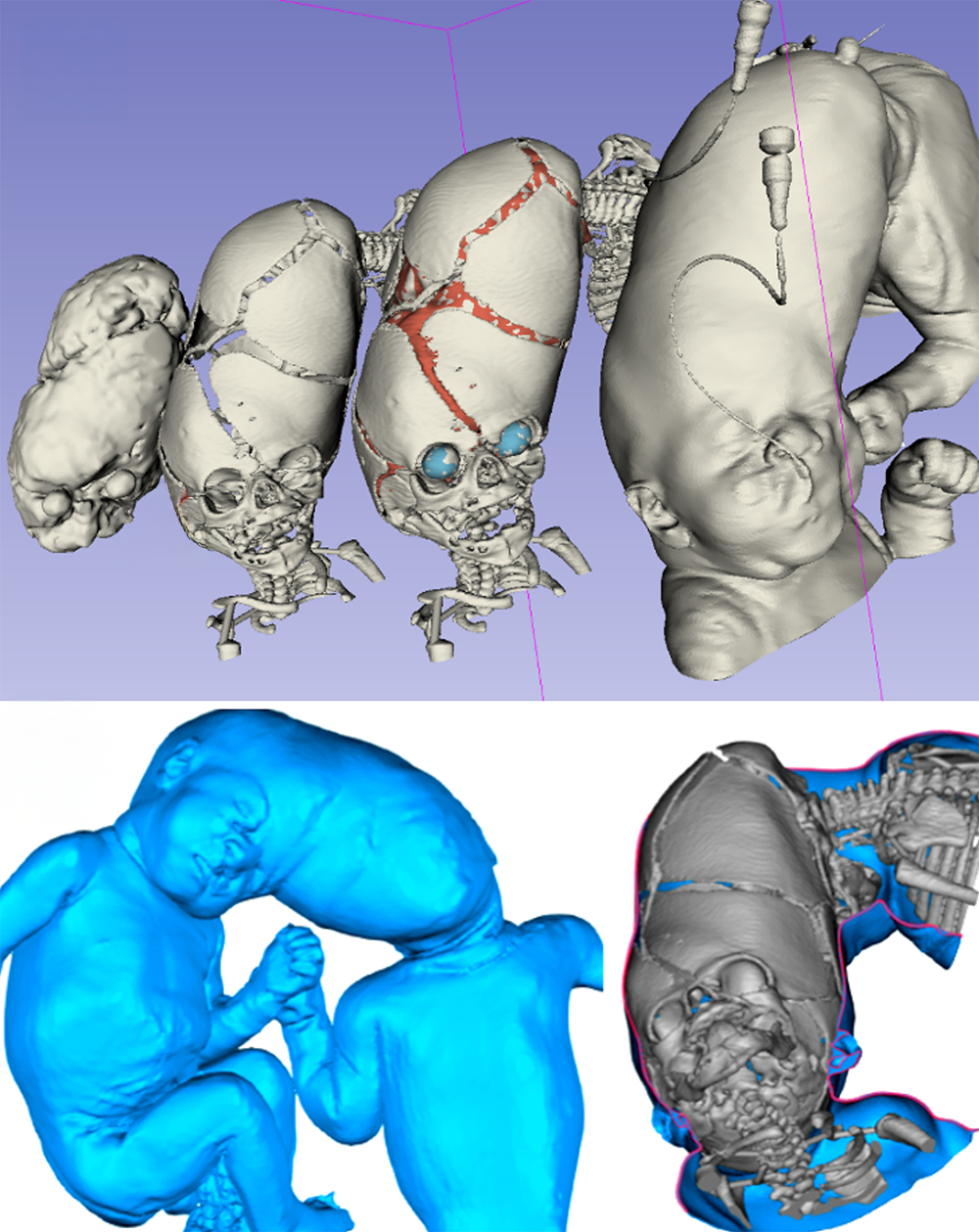
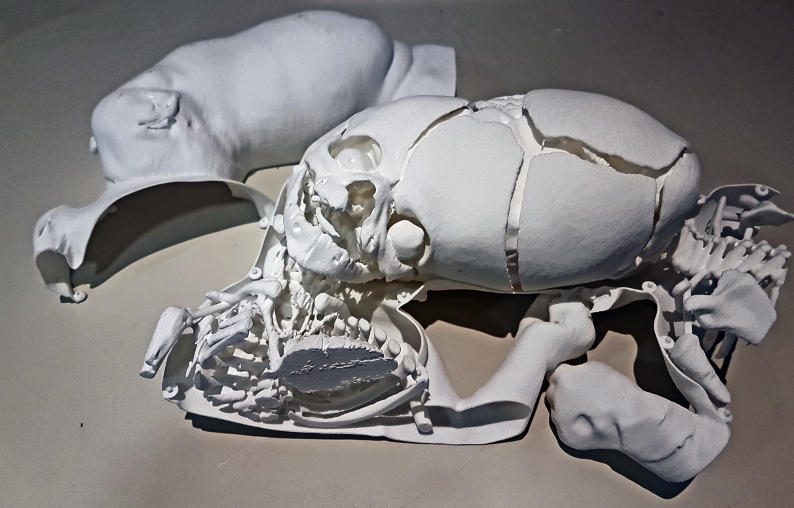
In this sort of malformation, given the complex, destructured and atypical anatomy, the use of 3D printed anatomic models is indispensable. These models provide the surgeon with a clear understanding of the surgical anatomy, which contributes to a good orientation for the team during the surgery. Therefore, we initiated the construction of these anatomic models through a partnership with Biodesign Lab Dasa/PUC-Rio. After the MRI, the 3D models were prepared.
Following the creation of the first anatomic 3D model and the performance of all the complementary exams necessary, we scheduled the first surgery, which took place in November 2019. I considered this surgery to be one of the most challenging, thereafter called the “fear breaker surgery”, due to it being the first case of such gravity, the greatest challenge being dealing with the unknown, as well as the enormous responsibility we had toward those parents.
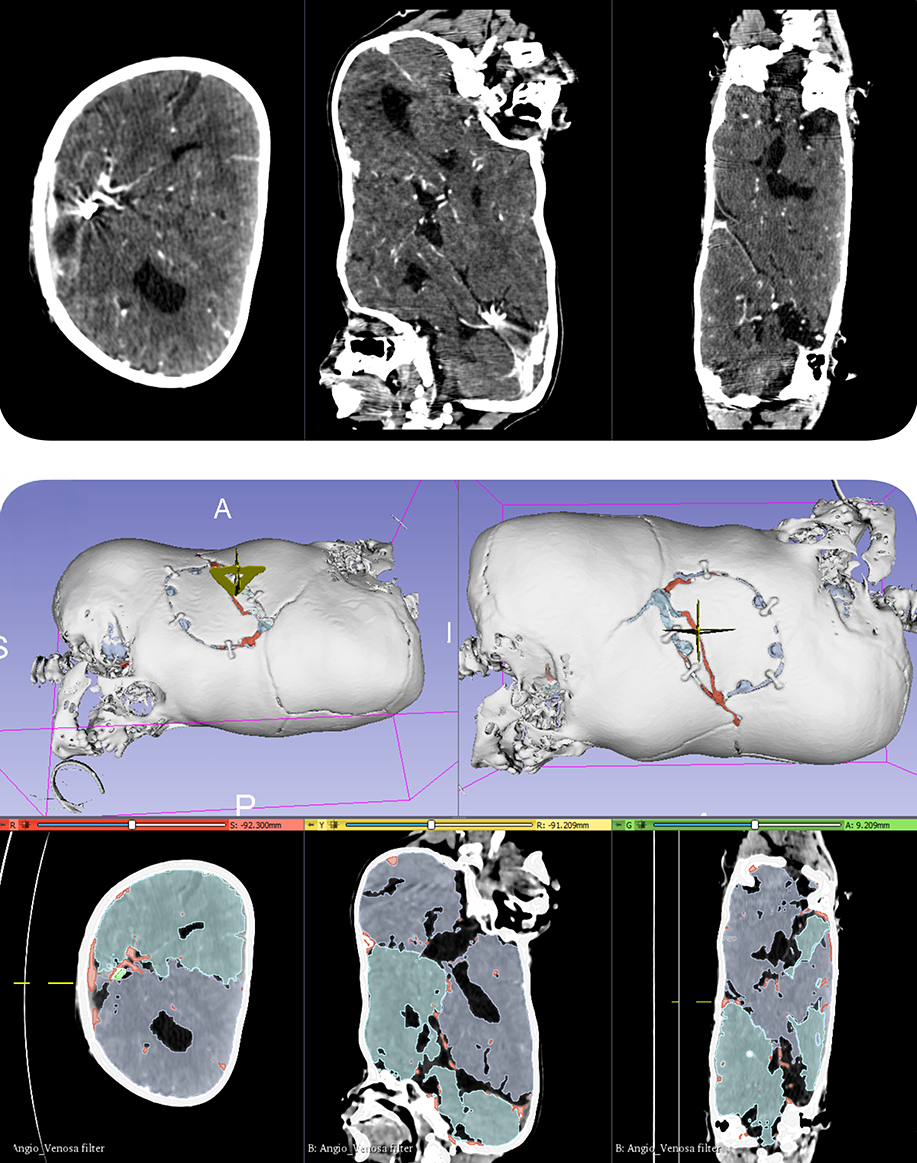
We scheduled the second surgery of partial separation juxtaposed to the first. This procedure took place two months after the first one. This waiting period between surgeries was necessary for the venous circulation to settle and for the development of a collateral venous circulation. After creating a new anatomic model, the surgical planning was established, with excellent progression of the hemispheric veins’ coagulation, which ran towards the circular sinus, obtaining good partial separation. The postoperative result was satisfactory, with the twins demonstrating excellent recovery, without any motor deficit, venous infarct, ischemia, or bleeding. A postoperative CT scan showed a good degree of separation.
We followed protocol and performed segmentary separations. Initially we scheduled four partial separations, followed by the disconnection; however, due to the complexity of the case we opted to further fragment the segments, and to date we have performed seven surgeries, without any interference. Between each procedure, new imaging exams such as MRI, CT scan, cerebral angiography were performed, and new anatomic 3D models were made. These exams and the 3D printing of the models are of extreme importance, for both the surgical planning and the visualization of the new collateral circulation established.
The final separation was scheduled for June 2022. In this procedure, the definitive separation of the twins was attempted, almost three years after the first one. It was a gift to this suffering family.
In February 2023, we received our second case of craniopagus at 13 weeks of gestational age. Another big challenge for us because, in addition to craniopagus, there was also a complex cardiac malformation (single ventricle) in one of the fetuses. We initiated an elaborate plan with a multidisciplinary group of specialists to develop a structure to begin the surgical process.
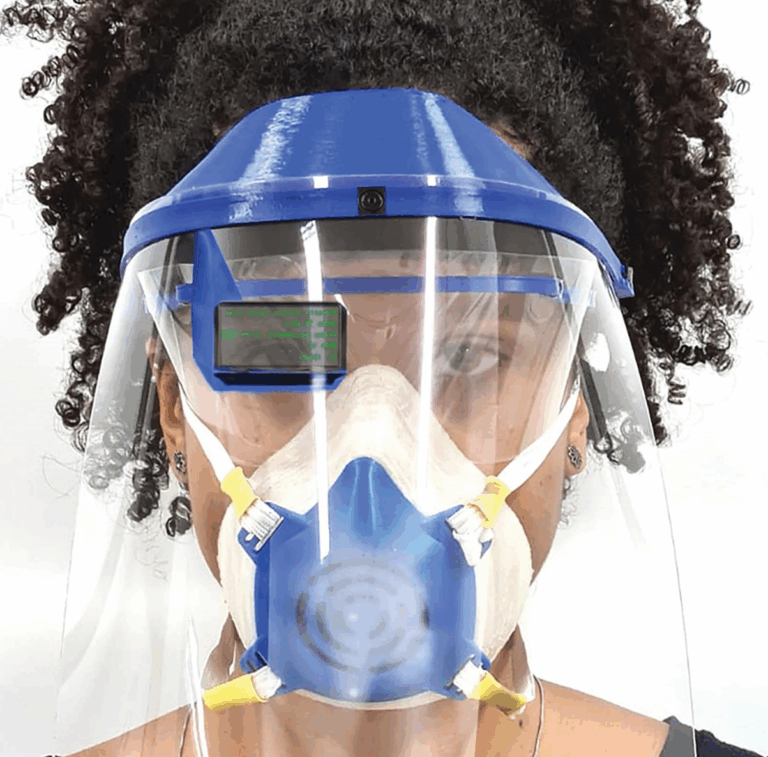
In this case, the surgical approach had to be performed in a single procedure due to the cardiac malformation. For the best possible planning, the use of 3D-printed anatomic models was indispensable, as well as discussions with Professor Owase Jeelani’s team using the metaverse.
After birth, at 32 weeks of gestation, new examinations were performed with CT and MRI. The twins were separated 52 days after birth. The neurosurgery was a success. The twin with the cardiac malformation did not survive, but he donated meninx, bone and skin to his brother who had an excellent clinical outcome.
Clinical Study 2
(Pediatric Surgery)
CONJOINED TWINS
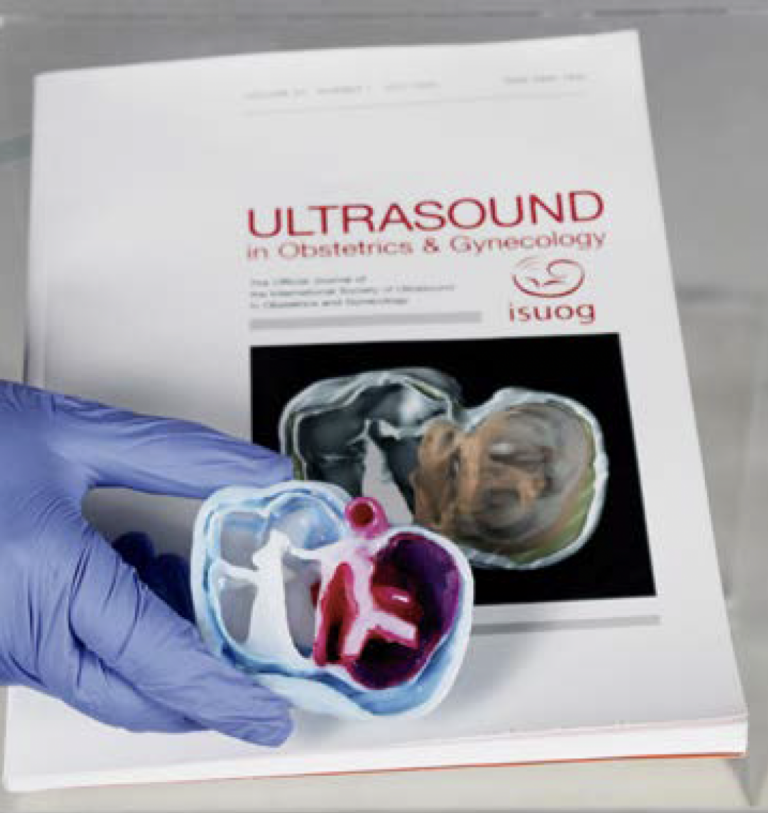
As a neonatal general surgeon, I have frequently worked with prenatal diagnosis and fully understand its crucial role in planning perinatal surgeries and follow-ups. In most cases, lesions are identified through routine obstetric ultrasound (US). However, magnetic resonance imaging (MRI) can provide a more detailed assessment. MRI serves as a complementary diagnostic modality, particularly in inconclusive cases that require further investigation. Unlike US, MRI is not affected by fetal position, oligohydramnios, bone interference, or maternal obesity.
One of the greatest challenges in pediatric surgery is the management of conjoined twins (CTs), a congenital anomaly associated with significant morbidity and mortality. CTs are classified based on their site of attachment, with ventrally fused twins being the most common. Among them, omphalopagus and thoracopagus are frequently observed. The extent of organ sharing, particularly cardiac involvement, determines the feasibility and prognosis of surgical separation. A meticulous preoperative evaluation, detailed planning, and a well-prepared multidisciplinary team are essential for a successful separation procedure.
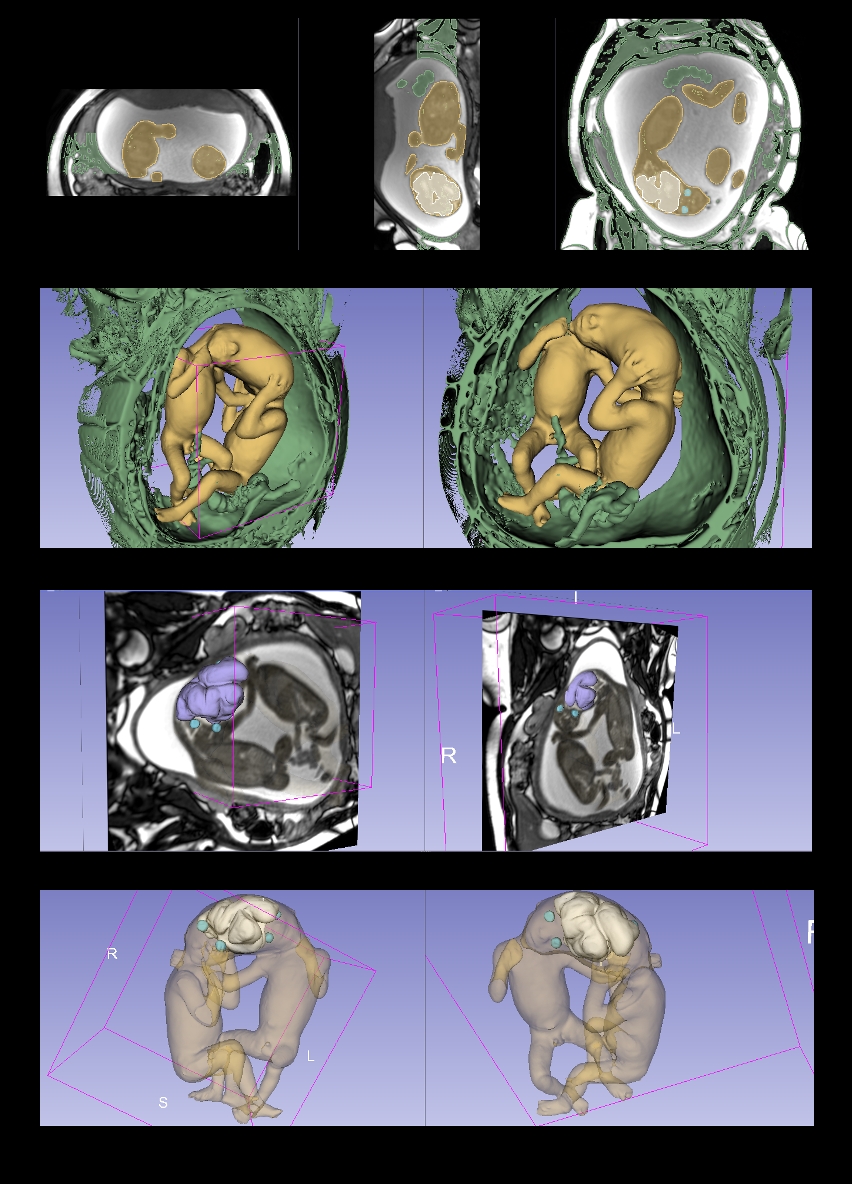
A 31-year-old G2P1 woman with a triplet pregnancy was referred for fetal MRI at 28 weeks of gestation. The fetuses were believed to be dichorionic and diamniotic, with a set of CTs fused at the abdomen. MRI was performed using a 1.5-T scanner, confirming the prior diagnosis of a normal singleton fetus alongside a pair of CTs. The fusion extended from the xiphoid process to the umbilical cord insertion (omphalopagus). Both livers were fused, but the intestinal loops and colons appeared normal. The gallbladders were identified and visualized.
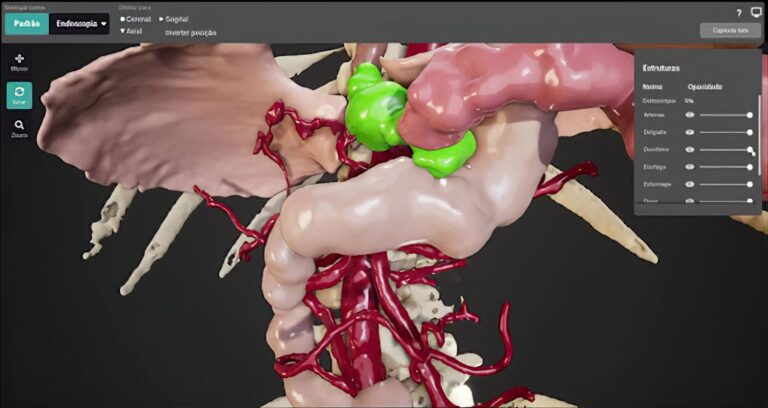
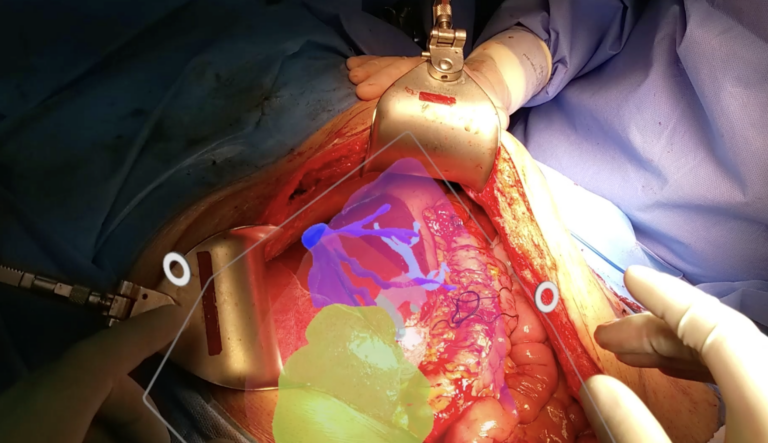
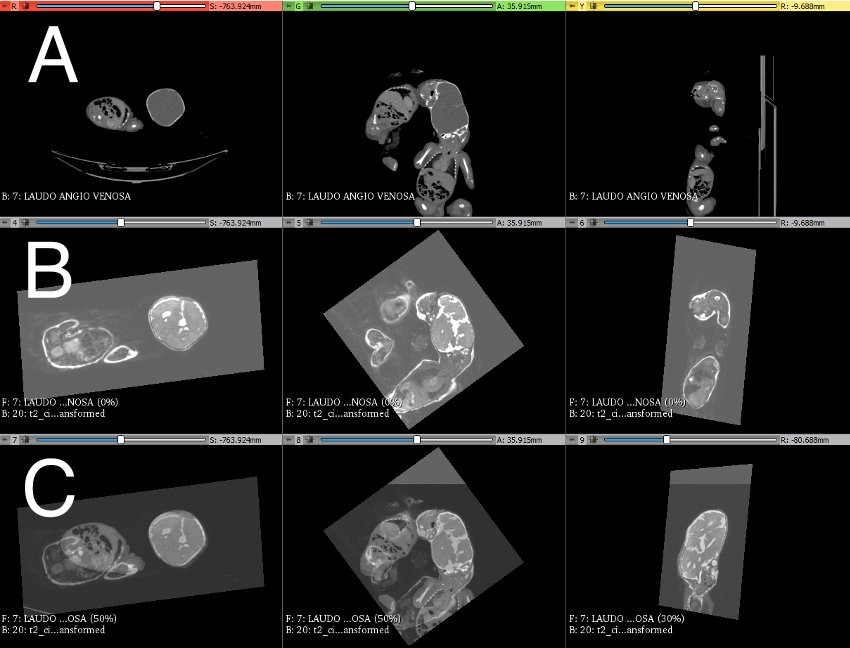
Following delivery at 35 weeks of gestation, further imaging studies were conducted. A computed tomography scan was performed, which confirmed hepatic fusion. The vascular connections of the liver were isolated and reconstructed in 3D, classifying the fusion as a type I hepatobiliary fusion. Immersive images were generated and exported, allowing for detailed preoperative and intraoperative analysis using the 3D Slicer application on mobile devices. The 3D reconstruction enabled the surgical team to meticulously study the vascular connections, facilitating surgical planning for separation.
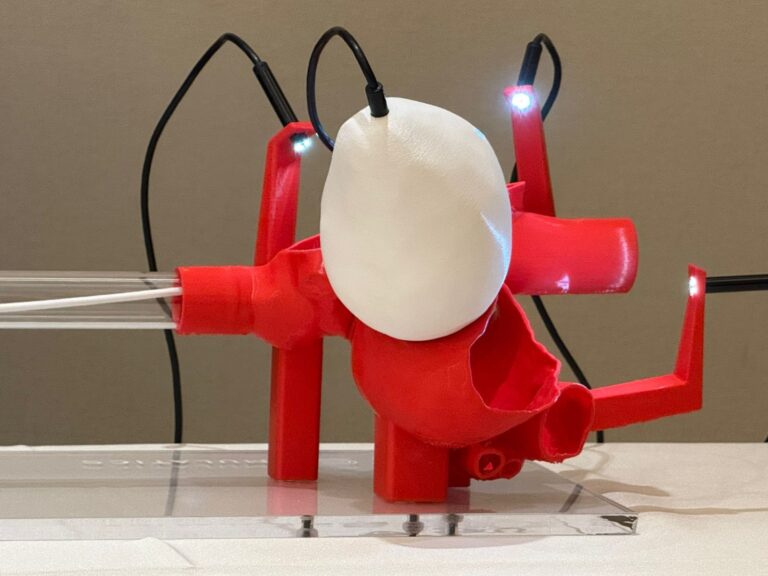
The separation of CTs requires a coordinated multidisciplinary effort to address the complex surgical and medical needs of these patients. A simulation-based approach was employed using preassembled mannequins replicating thoraco-omphalopagus twin anatomy. This simulation modality provided a safe training environment for a multidisciplinary team, including neonatologists, nurses, respiratory therapists, and surgeons to refine clinical decision-making, procedural strategies, and emergency management protocols. Simulation-based clinical rehearsals offer a valuable opportunity to prepare for rare, complex, and patient-specific procedures.
The surgical procedure was uneventful, and the patients remain under follow-up without any complications.