Congenital heart disease (CHD) is the most common congenital malformation, and an important cause of perinatal mortality and disabilities related to birth defects all over the world. The prevalence of CHD is 10 – 12 cases for every 1000 live births, most due to postnatal diagnosis of mild disease. The incidence in fetuses is even higher and estimated around 6,5%. Cardiac screening by ultrasound (US) evaluation of the fetal heart is the most important tool to maximize its prenatal diagnosis.
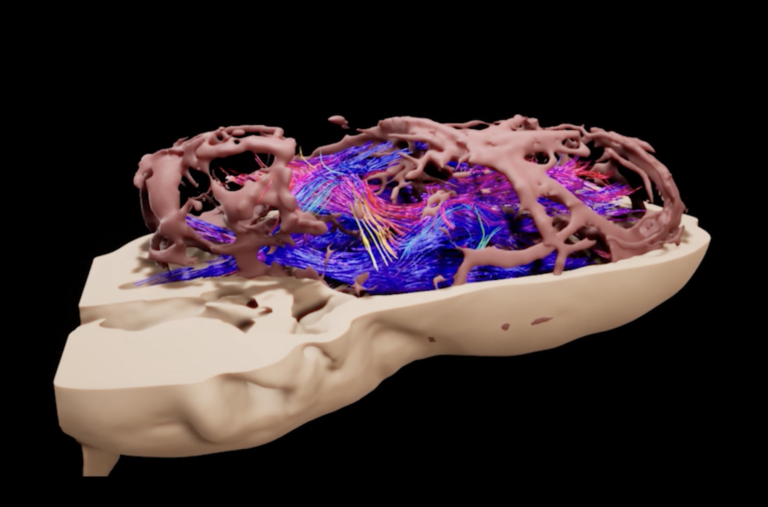
Advances in imaging techniques such as three-dimensional (3D) US have provided better accuracy of cardiac anatomy. 3D US with software spatio-temporal image correlation (STIC) allows the volume of the heart to be collected and analyzed in multiplanar and rendered modes.

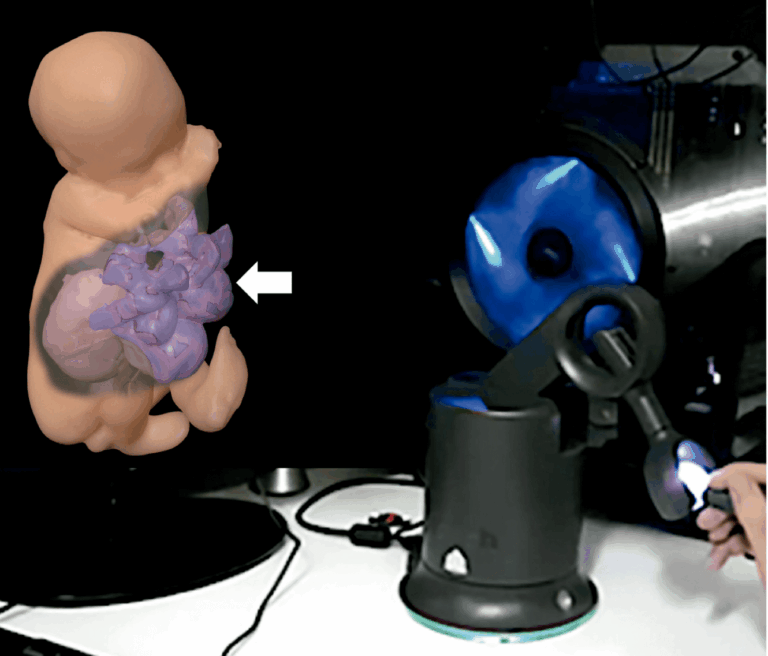
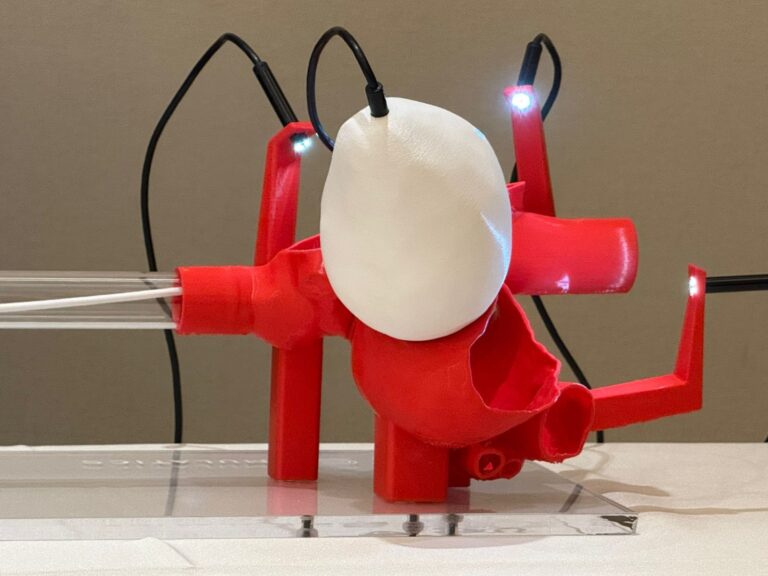
In the early 2010s, the emergence of 3D reconstruction software, combined with 3D printers, enabled virtual and physical reconstructions of fetuses, as well as virtual navigation of fetal cavities using 3D US and magnetic resonance imaging, enabling realistic visualizations of structures such as the airways, the urinary tract and the nervous system in cases of malformations. But only after the development of STIC, precise heart 3D images could be obtained.

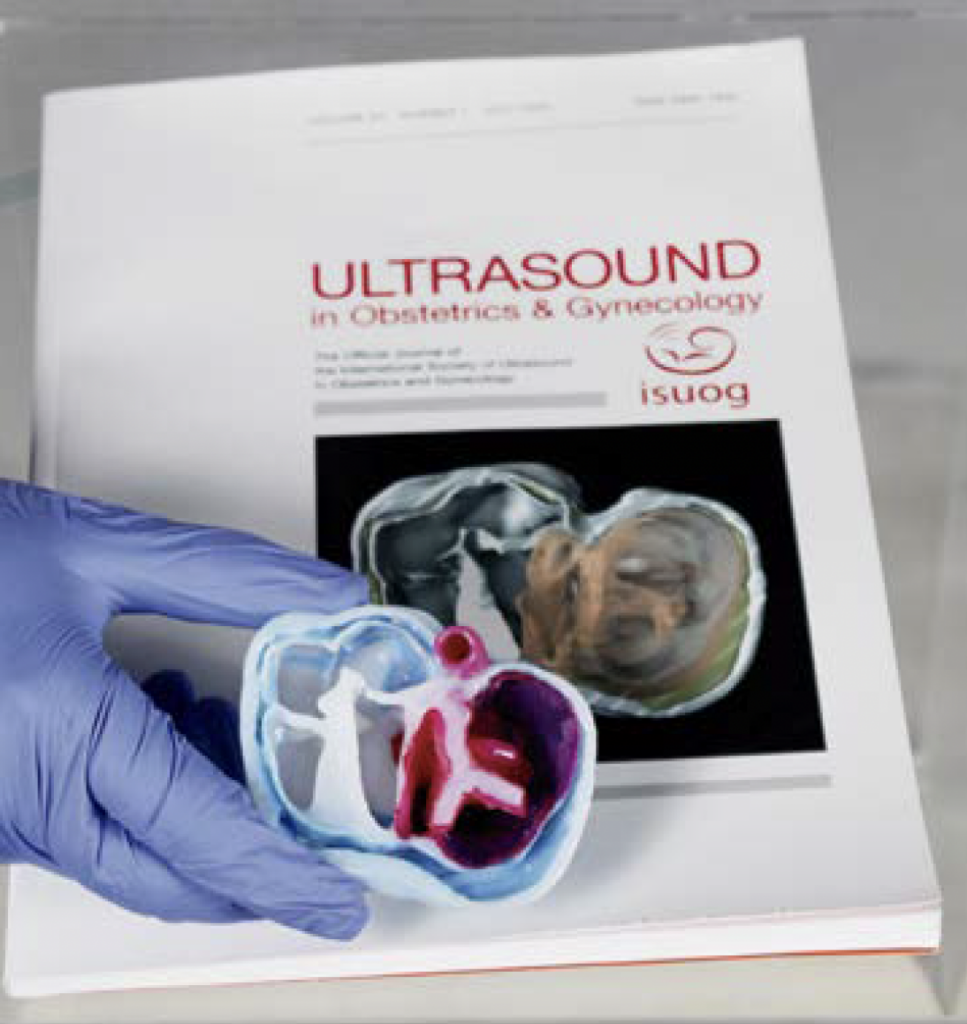
3D virtual and physical model of the fetal heart enables a better understanding of CHD improving parental counseling, teaching, as well as interactive discussions between the multidisciplinary medical team (maternal-fetal medicine specialist, neonatology, pediatric cardiology, and cardiovascular surgeon).
We studied the advantages of the use of physical models of fetal hearts with congenital heart anomalies to aid the understanding of these diseases by parents. After diagnosis, we offered an explanation to parents and their companions using 3D printed models. Finally, they answered a questionnaire about their feelings towards the fetal heart anomaly. Most of them declared that the physical model made them understand better the fetal condition, making them more self-assured and able to make decisions.

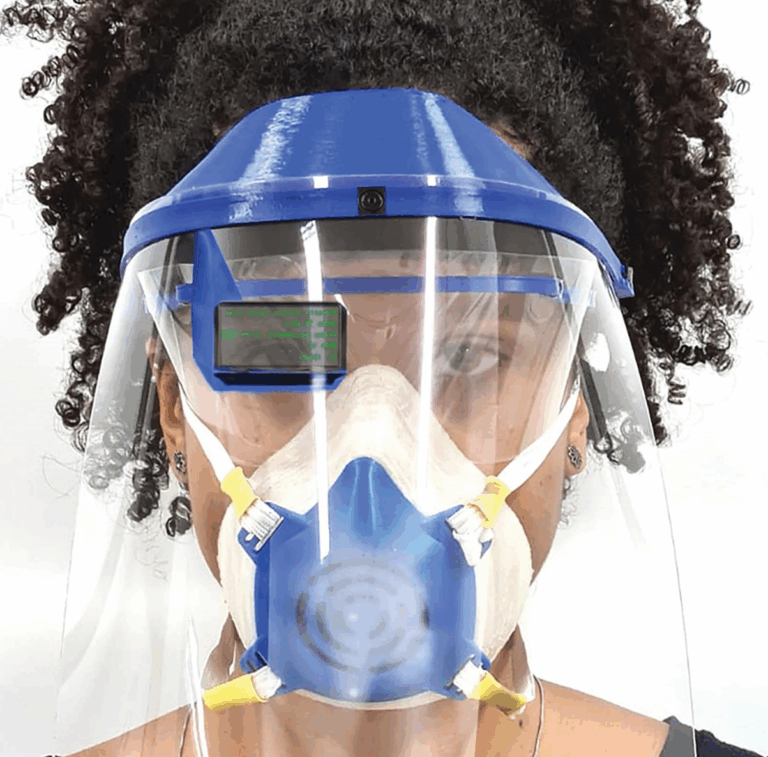
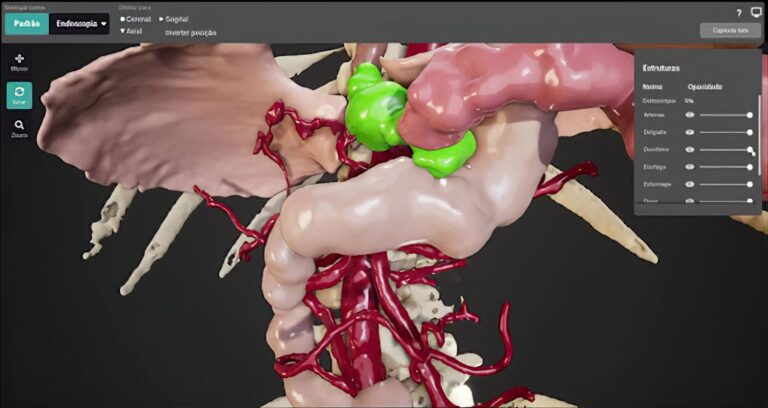
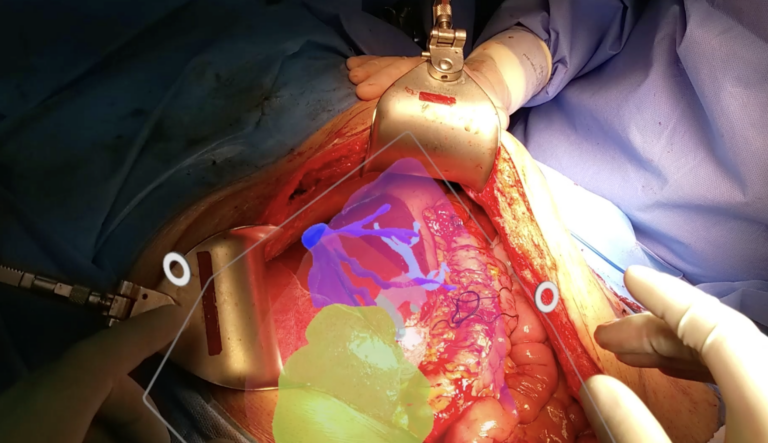
We did a pilot study using the platform called Elucis (Realize Medical, Ottawa Canada), for fetal heart segmentation. This system allowed a 3600 navigation and posteriorly utilizing in 3D printing, virtual reality and metaverse. Again, the visualization of normal fetal cardiac anatomy and its visualization enhanced education of students, residents and young professionals enrolled in fetal medicine.
Of course, these new technologies require a learning curve even for professionals with experience in congenital heart disease, design and the use of platforms. But the first step is the acquisition of one 3D volume from a four-chamber view of a fetal echocardiogram, that can be obtained from any equipment with STIC technology and a volumetric transducer.